Inviting comment on phase 3 COVID study vaccine trial design - with a focus on transparency and other guidelines that may foster finding reliable answers and trust among all stakeholders.
I’ve read the FDA guidance for vaccine trials and found it helpful to my understanding but questions remain. * https://www.fda.gov/media/139638/download
Specifically, I did not see criteria for when sponsors should do the analysis - to see if the 50% threshold for efficacy has been met.
Initial thought is that it should be event driven : a certain number of COVID cases, hospitalizations, ICU, and deaths in the study population triggers unblinding. Q1: If so, what might that magic number be in a 30,000 person RCT study?
Q2 Should every study vaccine sponsor agree to the same criteria? Doing so would be an incentive to enroll persons at higher risk of exposure and the worst outcomes in order to efficiently get to the finish line: mature outcome data.
Q3: If you had to choose one event as the trigger for unblinding, what would that be? I assume it should not be x number cases because an effective vaccine might not prevent infection so much as limit its severity.
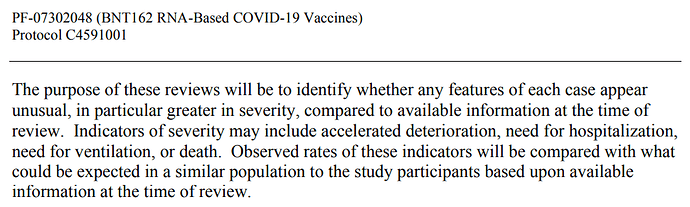
I suppose that interim safety monitoring by DSMB can call for unblinding at pre-specified intervals which might also inform if there are efficacy signals - that might trigger the company (if informed by the DSMB) to submit the findings to FDA. If this is the roadway to FDA submission, I’m worried. * Related DSMB background: https://www.fda.gov/media/75398/download
In summary, my assumption is that the number of COVID events to trigger unblinding should be pre-specified and explained to all stakeholders - in order to depoliticize vaccine research, limit gaming by sponsors, and foster public trust.
Q4 Is there some other way? What am I missing?
Added reference 4:25PM
Lancet: COVID-19 vaccine trials should seek worthwhile efficacy
Philip Krause Thomas R Fleming
Ira Longini Ana Maria Henao-Restrepo
Richard Peto for the World Health Organization Solidarity Vaccines Trial Expert Group † Published:August 27,
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31821-3/fulltext
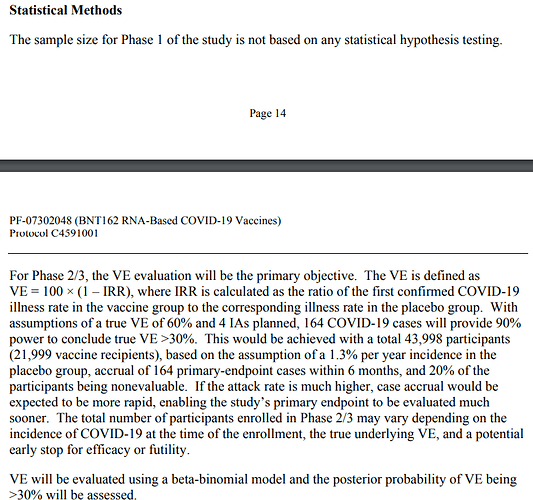
An answer comes with the publishing of the protocol by Pfizer:
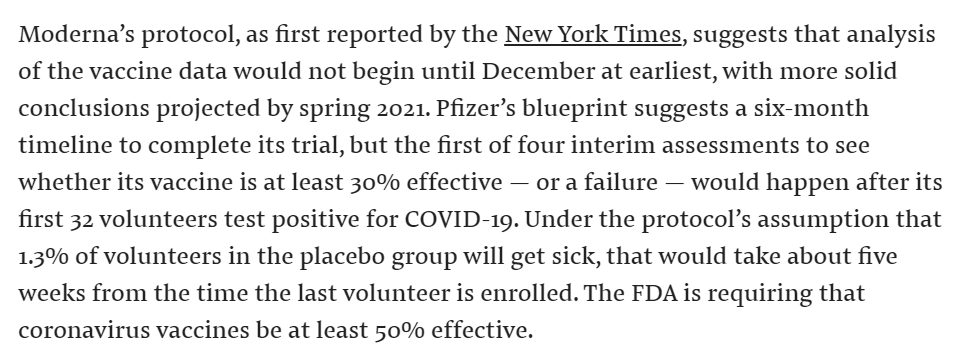
Added 9/18: Nice to see more public disclosures on COVID events that will trigger a Go/No go decision. This report based on the Moderna protocol
9/20: What ballpark number of COVID case, hospitalization, and death events would give you confidence that the study predicts meaningful benefit in the real world?
Assumption: harm from getting efficacy wrong includes false sense of security that could lead to more cases and deaths.